Congestive heart failure
Congestive heart failure or CHF, also known as heart failure, affects the heart’s ability to pump blood efficiently. It is a chronic progressive condition where the heart cannot pump blood as it should due to build of fluids in the heart. Read More
Top Doctors For Congestive heart failure Treatments
Top Hospitals For Congestive heart failure Treatments
Congestive heart failure
Table of contents
What is Congestive heart failure?
Congestive heart failure or CHF, also known as heart failure, affects the heart’s ability to pump blood efficiently. It is a chronic progressive condition where the heart cannot pump blood as it should due to build of fluids in the heart. Though it is called heart failure, it does not mean the heart has stopped working; instead, it shows that over time, the contracting ability of the muscles of the heart has reduced or the ability of the heart to pump blood has reduced due to a mechanical problem. And as a result of this, the heart becomes congested because the heart does not pump blood as fast as the blood returns to the heart; hence the heart is not able to meet up with the demand of the body, making it difficult for the organs of the body to get enough oxygenated blood.
There are four chambers of the heart, which include two atria (the atria collects blood as the blood circulates the body) which are in the upper half of the heart. The two ventricles (which pump blood to the organs and tissues of the body) are at the lower part of the heart. When the ventricles cannot pump enough blood, CHF develops, causing the fluid to build up in the liver, abdomen, lungs, and lower body.
To make up for this, the body adopts a compensatory mechanism. To use less time after contracting to refill, the heart beats at a faster rate. Still, in the long run, the blood that circulates is not much, and the heart palpitates as a result of the extra effort. This will cause fluid to fill the lungs causing shortness of breath. The kidneys may be affected as the kidneys may fail because enough blood doesn’t reach the kidneys; hence, sodium and water retention.

Types of CHF
There is the left-sided CHF and the right-Sided CHF. However, there is the possibility of having both types of CHF, usually starting from the left side and then moving to the right side.
- The right-sided CHF occurs when pumping blood to the lungs becomes difficult by the right ventricle. Fluid retention will be seen in the lower extremities, abdomen, and vital organs due to blood backup in the blood vessels.
- The left-sided CHF happens when blood is not pumped out properly to the body. Breathing becomes difficult as the condition progresses, and this is due to the accumulation of fluid in the lungs. This type of CHF is the most common type. There are two kinds of left-sided CHF
Diastolic heart failure, also known as diastolic dysfunction, occurs when the left ventricle’s muscles are stiff, and it cannot relax. And as a result, between beats, the heart can fill with blood.
Systolic heart failure happens when there is a failure of the left ventricle to contract normally, thereby causing a reduction in the force level required to push blood into circulation. The force is needed for the heart to pump correctly.
Stages of Congestive Heart Failure
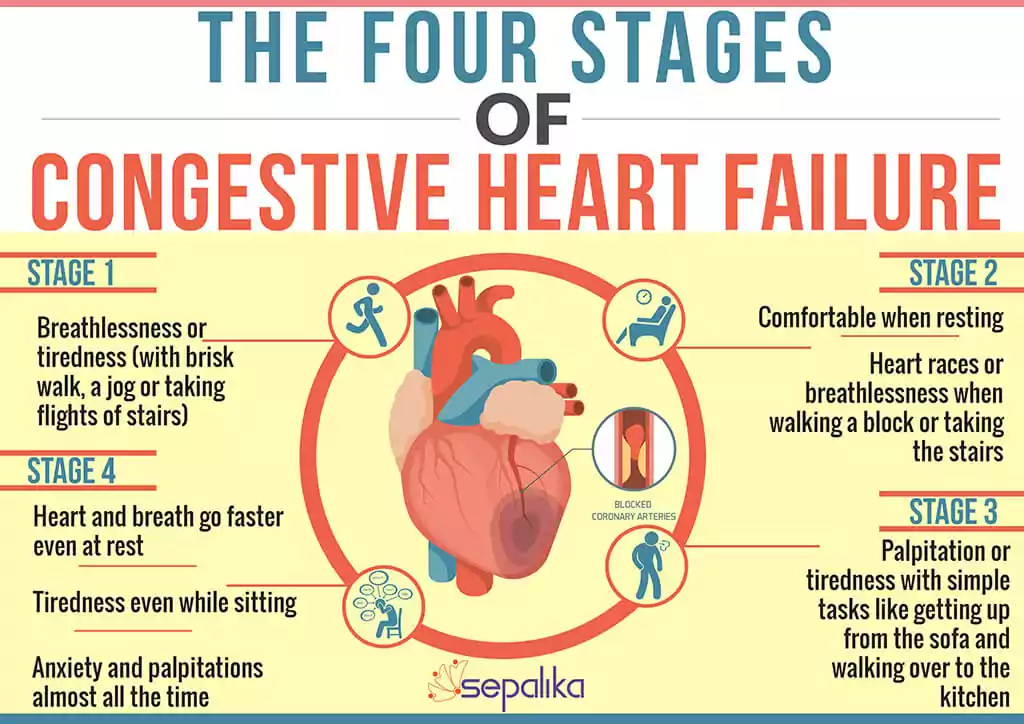
There are different stages classification by the American Heart Association (AHA) and American College of Cardiology (ACC), and the New York Heart Association (NYHA).
The clinical classification of heart failure by the New York Heart Association (NYHA) is done according to the degree or functional limits. It classified or ranked people as classes I to IV.
| Stages | Main symptoms | Outlook |
| Class 1 | During physical activity, no symptom is experienced | Through heart medications and monitoring, and lifestyle, CHF can be managed |
| Class 2 | One may experience fatigue, shortness of breath, and palpitations during regular physical activity, but one is most likely comfortable. | Through lifestyle, heart medications, and monitoring, CHF can be managed. |
| Class 3 | At rest, one is comfortable; however, there is a noticeable limitation of physical activity. Palpitations, fatigue, or shortness of breath may be felt even during mild exercise. | At this stage, it is advised to talk with your doctor for details on heart failure. Treatment at this stage can be complicated. |
| Class 4 | Symptoms are present at rest, and even when performing any physical activity, it is difficult to do so without symptoms. | At this, CHF has no cure. Palliative care and quality-of-life options will be of better use here. Discuss the risks and benefits with your doctor. |
The American College of Cardiology/American Hearts categorized individuals at risk of heart failure. It used letters A to D to categorize. Doctors use this classification method to spot risk factors and start treatment aggressively early enough to help delay or prevent heart failure.
- Stage A: in this stage, several risk factors predispose one to having heart failure, and they include high blood pressure, coronary artery disease, diabetes, metabolic syndrome, family history of myopathy, history of alcohol abuse, and no sign or symptoms of heart failure
- Stage B: There is heart disease but no symptoms. People in this stage have been diagnosed with systolic left ventricular dysfunction. Still, they have not yet had any symptoms, and they include those with valve disease, prior heart attack, and cardiomyopathy.
- Stage C: there is heart disease, and there are symptoms and signs of the disease. People who have already been diagnosed with systolic heart failure and have previously had or are presently having symptoms. Some of the common symptoms include fatigue, the ability to exercise is reduced, shortness of breath, Swollen ankles, feet, lower legs, and abdomen (edema).
- Stage D: the need for specialized care as heart failure is advanced. Systolic heart failure in patients and even after receiving optimum medical care, advanced symptoms are present.
Causes of Congestive Heart Failure
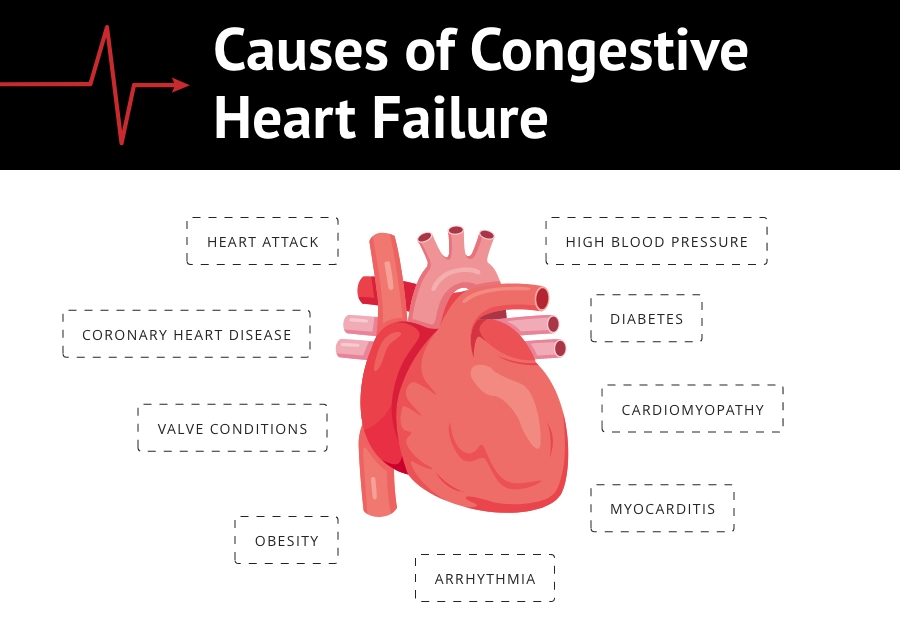
- Coronary artery disease: The coronary arteries are the arteries usually small in size that supplies blood to the heart. These arteries become blocked when cholesterol and other fatty substances block the arteries causing the arteries to be narrow, thereby restricting the flow of blood, which can damage the arteries.
- Heart attack: When the blood flow to the heart is stopped as a result of sudden blockage of the coronary arteries, a heart attack happens, and this will cause the heart muscle to be damaged. This will result in the area being scarred and preventing it from working correctly.
- Cardiomyopathy: There are other factors that cause damage to the heart muscle aside from blood flow artery issues like infections, drug abuse, or alcohol
- Hypertension or high blood pressure: A higher than normal blood pressure may cause someone to have CHF. One of the causes of hypertension is arteries hardening which will cause the pressure in the arteries to increase.
- Valve conditions: Blood flow through the heart is regulated by the valves. They do this by opening and closing the heart chambers to let blood in and out. A heart infection or defect can cause the valves not to correctly open and close, thereby causing the ventricles to do more work in pumping blood.
- Some allergic reactions and infections that are severe can be contributing factors to CHF.
Even though the heart-related disease can cause CHF, there are factors not related that can increase one’s risk of having heart failure, and they include:
- obesity
- certain drugs used during chemotherapy
- diabetes
- thyroid disease
- Some allergic reactions and infections that are severe can be contributing factors to CHF.
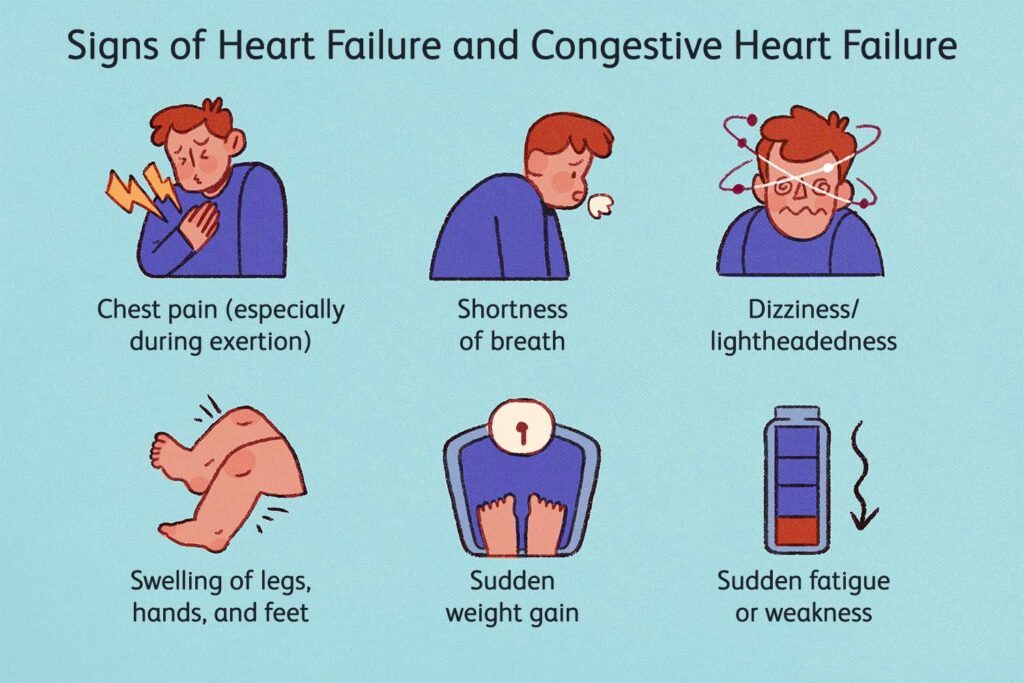
Symptoms of CHF
Sometimes one may have no symptoms, or the symptoms may be mild, but this does not mean that there is no heart failure. Heart failure symptoms may come and go and range from mild to severe. Over time, heart failure worsens with more or different symptoms.
Initially, one may not notice any symptoms, but specific symptoms will be noticed as the condition progresses.
At first, the following symptoms may be noticed
- mostly at night, there is an increased urge to urinate
- the legs, feet, and ankles are swollen
- there is weight gain
- fatigue
As the condition worsens, the following symptoms will be noticed
- wheezing
- cough resulting from congested lungs
- heartbeats that are irregular
- shortness of breath which may be an indication of pulmonary edema
These symptoms below may indicate that there is a severe heart condition.
- fainting
- Pain in the chest that radiates through the upper part of the body, and this may also be an indication of a heart attack.
- Breathing that is rapid.
- As a result of oxygen lack in the lungs, the skin may turn blue.
Treatment of Congestive Heart Failure
The goal of therapy for heart failure is to prevent deterioration of the condition that is reducing the need for hospitalization and death, improving the quality of life, and easing the symptoms.
With medication, lifestyle changes, or surgery, one’s condition can become better. The outlook of someone with CHF is dependent on whether there are underlying diseases like diabetes or hypertension and how advanced the CHF is. The outlook improves if the condition is diagnosed early.
Some of the medications used include:
- Blood vessel dilators
- Dioxin
- Beta-blockers
- Calcium channel blockers
- Diuretics
- Angiotensin II receptor blocker
- Aldosterone antagonists
- ACE inhibitors (angiotensin-converting enzyme inhibitors)
When there is a need for cardiac implant devices, surgery may be recommended. These cardiac devices may be recommended to treat a problem that caused heart failure.
Preventive measures
There are things that can be considered, especially with lifestyle modification, to help reduce the risk of having heart failure or delay onset.
- Try to quit or avoid smoking.
- To maintain a well-balanced diet, it should include vegetables, whole grains, fruits, and proteins. You should try to avoid salt, sugar, fats that are solid, and grains that are refined.
- Exercise is also good for the body. Exercise can help to improve the health of the heart. Some suitable forms of exercise include bicycling, walking, and swimming.
- It is essential to be conscious of your weight. Being overweight or obese can affect the heart adversely. It is necessary to exercise and have a healthy diet regularly.
- Take alcohol in moderation.
- Keep away from drugs that are illegal.
- Ensure to stick to instructions for drugs prescribed
- Ensure to take medications if currently on medications for heart disease, diabetes, or hypertension.
Reference
- https://www.webmd.com/heart-disease/guide-heart-failure
- https://my.clevelandclinic.org/health/diseases/17069-heart-failure-understanding-heart-failure
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/congestive-heart-failure-prevention-treatment-and-research
“Medical Advice Disclaimer:
DISCLAIMER: THIS SITE DOES NOT PROVIDE MEDICAL ADVICE OR OPINION:
The information provided in this article or website by way of text, illustration, graphics, Images or any other form in this article or website is provided for informational purposes only. No information or material provided on this site is meant to be a substitute for a professional medical advice. Please refer to your family doctor or specialist in that field for any medical condition, diagnosis and treatment. Do not delay in contacting a professional on account of something you have read in this article or on this website.”