Lymphangiectasia
Lymphangiectasia is used to describe the dilation of the lymph vessels, especially in the intestine, leading to intestinal lymphangiectasia. It occurs as a result of lymphatic damage due to external causes. The symptoms range from mild to severe and can lead to complications. What is Lymphangiectasia? Lymphangiectasia is used to describe the dilation of the […] Read More
Top Doctors For Lymphangiectasia Treatments
Top Hospitals For Lymphangiectasia Treatments
Lymphangiectasia
Table of contents
What is Lymphangiectasia?
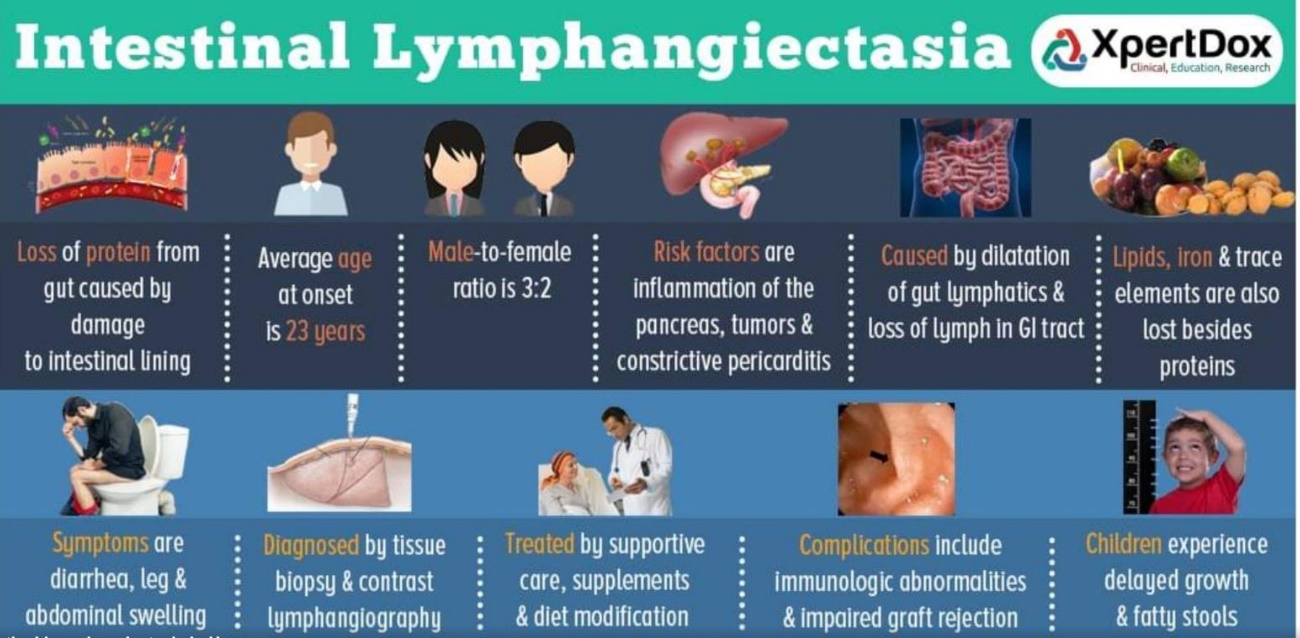
Lymphangiectasia describes the dilation of the lymph vessels, especially in the intestine, leading to intestinal lymphangiectasia.
Lymphangiectasia occurs as a result of lymphatic damage due to external causes, which could result in the blockage of lymphatic drainage, making the lymph rupture and split its content into the colon. It occurs in adults due to late sequels of mastectomy and radiation therapy.
What is intestinal lymphangiectasia?
Intestinal lymphangiectasia is a rare condition in which protein-losing gastroenteropathy involves dilatation of the intestinal lymphatics and loss of lymph fluid into the gastrointestinal tract, resulting in the conditions such as:
- the hypoproteinemia-low protein contained in the body,
- edema,
- lymphocytopenia-decrease in white blood cells in the blood,
- hypogammaglobinemia; low immunoglobulin G in the blood and
- immunologic anomalies.
Intestinal lymphangiectasia is generally diagnosed before one is up to 3 years but may be found in older patients. Prevalence is still unknown, but it has its main symptom, predominantly bilateral lower limb edema.
What are the types of intestinal lymphangiectasia?
- Primary intestinal lymphangiectasia,
It is also called “Waldmann’s disease.” When the abnormality of the lymph vessels of the intestine occurs in children. It could be congenital as it could result from improperly formed intestinal lymph vessels or blockage of lymph flow from the intestines.
- Acquire intestinal lymphangiectasia
It is mostly found in adults. One is not born with it, but it could occur due to certain external causes such as amyloidosis.
Causes
The causes of lymphangiectasia include:
- Congenital factors
- Mechanical processes and infiltration such as malignancy and amyloidosis
Symptoms
The symptoms of lymphangiectasia include:
In children:
- Edema: moderate or severe.
- Pericarditis or chylous ascites-stiffening of the sac that envelops the heart.
- Fatigue.
- Abdominal pain, with abdominal mass, which can be felt in the upper part of the stomach.
- Weight loss.
- Inability to gain weight.
- Moderate diarrhea and fat-soluble vitamin deficiencies due to the inability to absorb nutrients properly.
- Hypocalcemia-low calcium in the body, leading to convulsions.
In adults, it could also include some symptoms such as:
- Osteomalacia, vitamin D deficiency.
- Iron deficiency with anemia occurs due to multiple small intestine ulcers.
- Malabsorption syndrome can be found.
- Edema.
- Inflammation of the pancreas (pancreatitis).
How is lymphangiectasia diagnosed?
This condition could be diagnosed using:
- A blood test to ascertain protein levels in the blood.
- Computerized tomography (CT) scan.
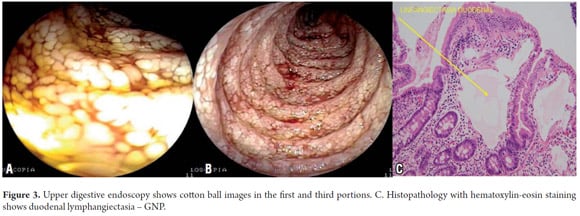
- Biopsy from the small intestine’s lining reveals the rupture and state of the lymphoid vessels.
- Endoscopic examination.
- Lymphoscintigraphy can be done.
Treatment
After finding out the main cause of the disorder, treatment can involve:
- High-protein diet
- Low fat with medium-chain triglycerides and other supplements such as antiplasmin, octreotide, etc., are also given to aid in managing symptoms.
- Surgery is recommended in extreme cases.
- Sometimes albumin infusion is done.
- Corticosteroid is also administered.
What are the complications of lymphangiectasia?
Complications include:
- Malignant transformation or lymphoma.
- Multiple cutaneous warts in association with lymphoma.
- Risk of infection.
- Gelatinous transformation of the bone marrow.
FAQ
Lymphangiectasia, unfortunately, has no cure yet but is being managed with dietary restrictions, involving a low-fat diet and supplementation of a specific type of fat that could be more easily absorbed by individuals with this disorder.
Conjunctival lymphangiectasia can be described as the obstruction of lymphatic channels, with the actual cause often unknown. Here, the conjunctiva is chronically swollen.
Protein-losing enteropathy (PLE) happens when albumin and other protein-rich substances leak into the intestine. Albumin, which contains much protein in the blood, serves in transporting hormones and retaining water in the blood.
The test for protein loss enteropathy can be done using Alpha 1 antitrypsin (A1AT), an intestinal clearance. It is the most common test performed in diagnosing protein-losing enteropathy. It has a high molecular weight but is minimally degraded in the gut and is excreted intact. Its clearance is calculated after 24 hr stool.
Lymphangiectasia is not contagious. It is caused by either congenital factors or mechanical processes such as amyloidosis.
Picture Courtesy: intestinal lymphangiectasia