Adenocarcinoma Renal
Adenocarcinoma renal refers to cancer that begins in the lining of the tiny tubes in the kidney that in waste removal and filtration. Renal cell adenocarcinoma is the most common type of kidney cancer in adults. It is also called hypernephroma, renal cell cancer, and renal cell carcinoma. Renal cell carcinomas (RCCs) which originate within… Read More
Top Doctors For Adenocarcinoma Renal Treatments
Top Hospitals For Adenocarcinoma Renal Treatments
Adenocarcinoma Renal
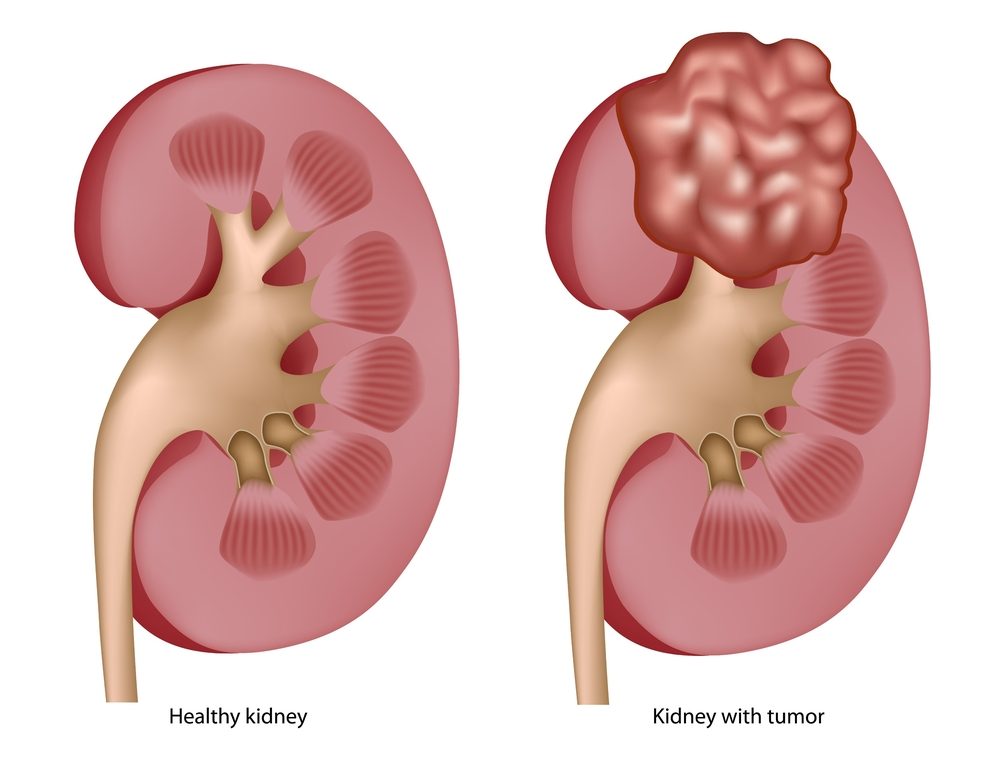
Adenocarcinoma renal refers to cancer that begins in the lining of the tiny tubes in the kidney that in waste removal and filtration. Renal cell adenocarcinoma is the most common type of kidney cancer in adults. It is also called hypernephroma, renal cell cancer, and renal cell carcinoma. Renal cell carcinomas (RCCs) which originate within the renal cortex, are responsible for 80% to 85% of all primary renal neoplasms.
What are the Causes and Predisposing Factors for Adenocarcinoma Renal?
Although research has not been able to point to the exact cause of adenocarcinoma renal, the following factors increase a person’s risk for renal cancer:
- Age: Adults between 50 and 70 years are more likely to have renal adenocarcinoma.
- Obesity: Overweight and obese individuals are prone to renal adenocarcinoma as opposed to their counterparts.
- Hypertension
- Chronic renal failure
- Dialysis treatment: This can cause acquired cystic kidney disease and in turn increases the chances of renal cell carcinoma.
- Polycystic kidney disease
- Race: Blacks are more likely to develop renal cell cancer, unlike whites.
- Sickle cell disease
- Renal stones
- Diseases: Disease conditions such as tuberous sclerosis, Von Hippel-Lindau syndrome, Birt-Hogg-Dube syndrome, hereditary papillary renal carcinoma, and hereditary leiomyomatosis and renal cell carcinoma (HLRCC) are all predisposing factors to the development of adenocarcinoma renal.
- Chemicals and substances: Exposure to certain chemicals and substances such as cadmium, herbicides, asbestos, and trichloroethylene.
Symptoms of Renal Adenocarcinoma
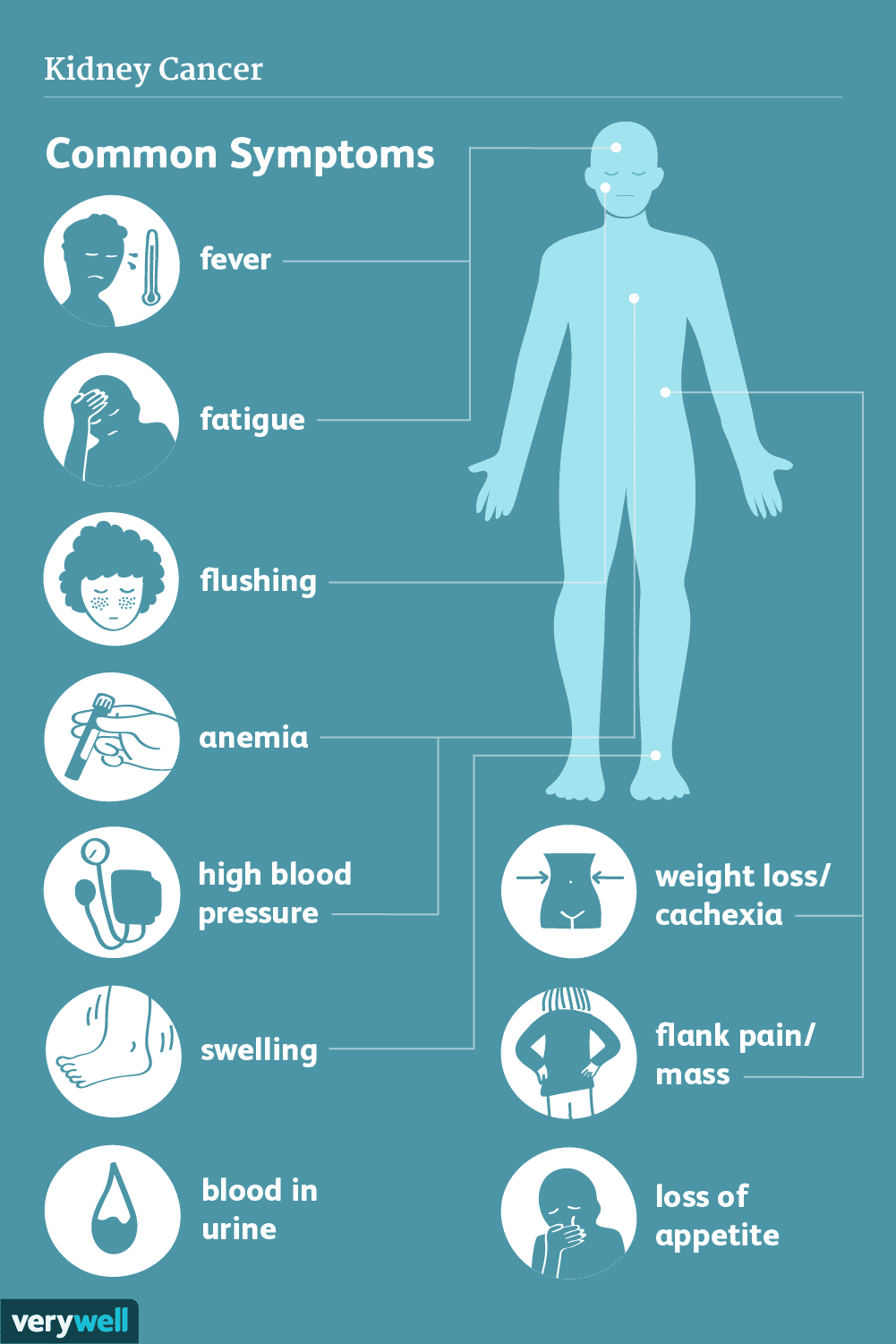
During the early stages, the patient is usually asymptomatic. This is because significant damage has yet to occur in the kidney. As the mass grows, symptoms may include:
- Hematuria (blood in the urine)
- Back pain (around the lower back and usually on one side)
- Flank mass (usually felt on palpation of the flank)
- Fatigue
- Hypertension
- Unexplained weight loss
- Anemia due to the inability of the kidney to produce erythropoietin, a precursor in red blood cell production.
- Fever
- High serum calcium level.
Flank pain, flank mass, and hematuria are usually seen in advanced cases and only occur in about 10% of early cases.
Diagnosis of Adenocarcinoma Renal

Following a report of the above clinical signs, a complete blood count and serum analysis is conducted after a thorough anamnesis and physical examination. A urinalysis is also performed, and cancer cells may be detected in some cases.
Renal and bladder ultrasonography is typically the first radiographic test performed when RCC is suspected. If the renal ultrasound shows a solid mass or a complex cyst with nodules, then a CT scan of the kidneys, ureters, and bladder should be done. It is necessary to perform the test with and without an IV contrast with delayed imaging of the entire abdomen and pelvis.
If the renal ultrasound is negative, but the patient has unexplained hematuria, a CT scan before and after IV contrast should be the next test as small solid renal masses can be easily overlooked on ultrasound, and small renal stones can also be overlooked.
A CT scan is used to stage cancer and detect lymphadenopathy and invasion of the renal vein, inferior vena cava, or adjacent organs. A CT scan can detect metastatic disease to the bones of the abdomen and pelvis only. The best test to find bone metastases is a whole-body bone scan.
An abdominal MRI can yield the same results as a CT scan for diagnosing and staging RCC but is more subject to limitations such as respiratory motion artifact because the images take longer to acquire.
Biopsies of the kidney can be obtained for cytologic and histologic examination. In certain instances, partial or total nephrectomy can also be performed to determine the presence or absence of renal adenocarcinoma.
Differential Diagnosis of Adenocarcinoma Renal
The differential diagnosis of renal adenocarcinoma includes the following:
- renal oncocytoma,
- multilocular cystic nephroma,
- lipid-poor renal angiomyolipoma,
- renal metastases,
- renal lymphoma, and
- solitary fibrous tumor.
Other renal abnormalities that can be confused with RCC include a prominent column of Bertin, renal infarct, renal abscess, and complex renal cyst. The finding of a renal infarct is usually associated with vascular abnormalities like renal vein thrombosis. The renal abscess typically has other clinical findings such as pyelonephritis, high white blood cell (WBC) count, fever, and chills while a complex renal cyst can be differentiated from a renal adenocarcinoma by radiologists through the Bosniak classification.
Treatment of Adenocarcinoma Renal
There are a few different ways to treat renal cell carcinoma. The decision on which method(s) is dependent on the age, health status, and stage of the cancer. The available options include:
Surgery:
Surgery is usually the first course of treatment for kidney cancer. If the cancer is confined to the kidney, this may be the only treatment needed. Additional treatments are recommended if it has spread to other organs and tissues. Surgery aims to eliminate the tumor while maintaining healthy kidney function. Different surgical procedures used to manage renal adenocarcinoma are:
- Radical nephrectomy: It involves the removal of the affected tissues and a large amount of healthy surrounding tissues. It could be done through a laparoscope-aided surgery in which multiple small incisions are made, and the laparoscope camera and surgical instruments passed through the holes. It can also be done as an open surgery depending on the size and location of the tumor on the kidney.
- Partial nephrectomy: This is called a kidney-sparing or nephron-sparing surgery. This is done to prevent future kidney-related issues. It removes the tumor and a few healthy tissues. Like total nephrectomy, it can be done as a laparoscopy or open surgery. It is preferred to a radical nephrectomy.
Nonsurgical treatments:
Nonsurgical methods are sometimes used to eradicate small kidney malignancies. These procedures are used in people who are not fit for a surgical procedure. These options are:
- Cryoablation: This is a treatment to freeze cancer cells. During cryoablation, a special hollow needle is guided with ultrasound and inserted through the skin and into the kidney tumor. Using a cold gas in the needle, the cancer cells are rendered inert.
- Radiofrequency ablation: It involves the use of heat to kill the cancer cells. Ultrasound or other imaging is used as a guide to insert a particular probe into the kidney tumor through the skin. The cancer cells are exposed to an electrical current through the needle, which causes them to heat up or burn.
- Chemotherapy: This includes drugs used to treat cancer and targeted therapy. Targeted drug therapies focus on certain flaws that are common in cancer cells. They include drugs such as bevacizumab, axitinib, lenvatinib, sorafenib, etc.
- Immunotherapy: Immunotherapy interferes with the ability of cancer cells to mimic normal body cells and evade destruction by the immune system.
- Radiation therapy: High-powered energy beams from sources like X-rays and protons are used in radiation treatment to kill cancer cells. In some cases, radiation therapy is used to control or lessen kidney cancer symptoms that have progressed to the bones and the brain.
Conclusion
The prognosis of kidney adenocarcinoma is dependent on the stage of the cancer, health status, and age of the patient. It is worthy of note that adequate discussions should be made with the physician to ensure that the patient is aware of possible side effects and demerits of each treatment plan.